
So much for vaccine-generated herd immunity
In an Israeli hospital outbreak, 96% vaccination rates (and universal masking) made no difference. And guess who had mild cases? Hint: not the vaccinated.
by Alex Berenson Oct 3, 2021
A reader tipped me to this fascinating paper in a peer-reviewed journal about a Covid outbreak in Israel that began in mid-July, just as vaccine failure was accelerating there.
A vaccinated dialysis patient was admitted to Meir Medical Center – a large Israeli hospital near Tel Aviv – with fever and cough. He remained on the dialysis unit for days, as his condition worsened. (One of many problems with overselling the vaccines is that it led to mistakes like this.)
By the time he was diagnosed with Covid-19, he had infected three fellow patients. He also had a PCR threshold of 13.6 – almost impossibly low, showing viral loads roughly 1 million times those in a lightly infected person. He was moved to a Covid-19 ward, where he eventually died (I say he, though the patient’s gender is not revealed; the paper refers to “they).
The paper, published in Eurosurveillance, a journal published by the European Centers for Disease Control, explains that the outbreak rapidly spread among both patients and staff of the hospital’s dialysis unit, the Covid-19 ward, and other wards. At the time, 238 out of 248 of exposed patients and staff had been fully vaccinated with Pfizer’s mRNA vaccine.
Again, the fact that 96 percent of the people in this population had been vaccinated – a level far above early estimates of the percentages required for herd immunity – apparently made no difference.
Further, all patients and staff were required to wear surgical masks when they were in the same room, and staff on the Covid-19 unit wore N95 masks and face shields.
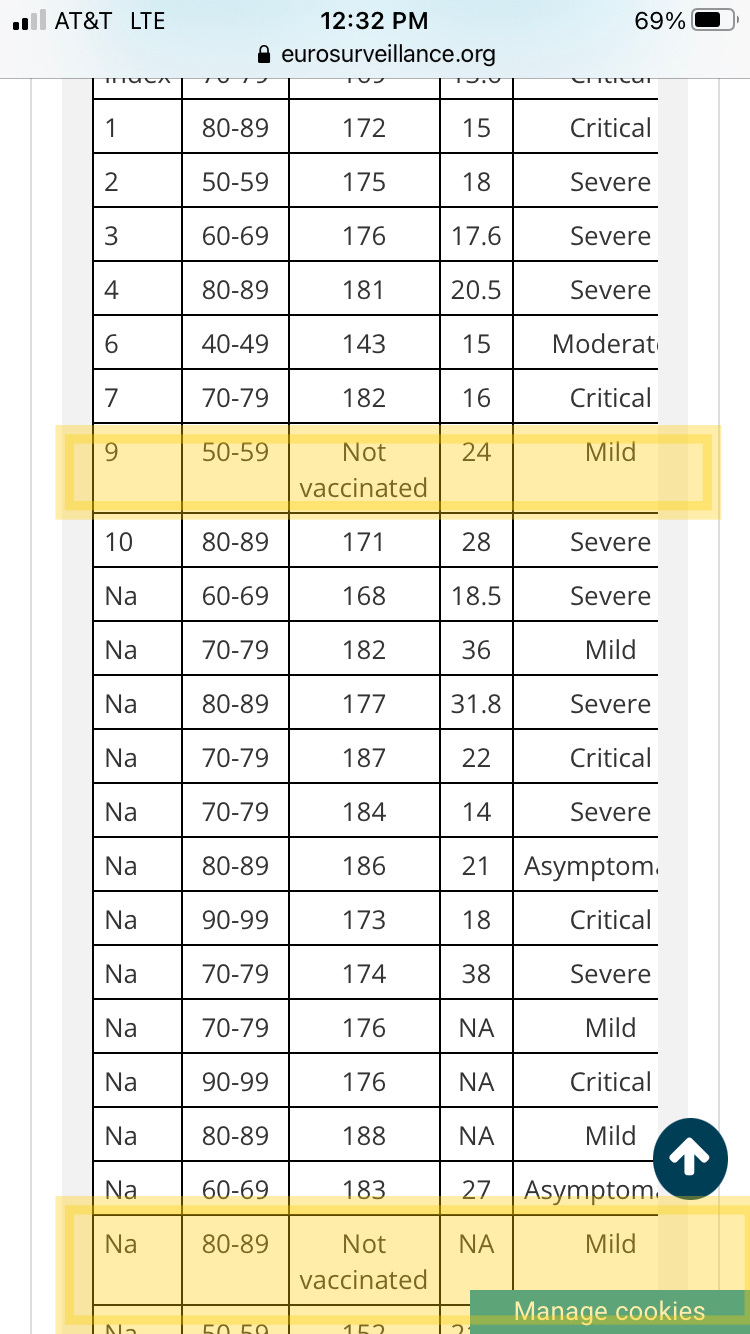
Ultimately, 39 out of the 238 exposed vaccinated people (16 percent) were infected, along with 3 out of 10 unvaccinated people – a difference that doesn’t reach statistical significance because the unvaccinated group is too small.
Of the infected, 23 were patients and 19 staff. The staff all recovered quickly. But five patients died and another nine had severe or critical cases. All were vaccinated. The two unvaccinated infected patients both had mild cases.
As the authors explained:
This communication… challenges the assumption that high universal vaccination rates will lead to herd immunity and prevent COVID-19 outbreaks… In the outbreak described here, 96.2% of the exposed population was vaccinated. Infection advanced rapidly (many cases became symptomatic within 2 days of exposure), and viral load was high.
SOURCE:
eurosurveillance.org/content/10.2807/1560-7917.ES.2021.26.39.2100822#html_fulltext



0 Comments